Spinal anesthesia is a widely used neuraxial technique that involves injecting local anesthetics into the cerebrospinal fluid, providing effective anesthesia for surgeries below the umbilicus. This method is particularly valuable for procedures such as cesarean sections, orthopedic surgeries, and urological interventions. The popularity of spinal anesthesia stems from its numerous advantages, including reduced risks of respiratory complications, avoidance of general anesthesia, and enhanced postoperative pain control. The duration of spinal anesthesia is a critical factor in its clinical utility, influenced by a complex interplay of pharmacological, procedural, and patient-related factors.
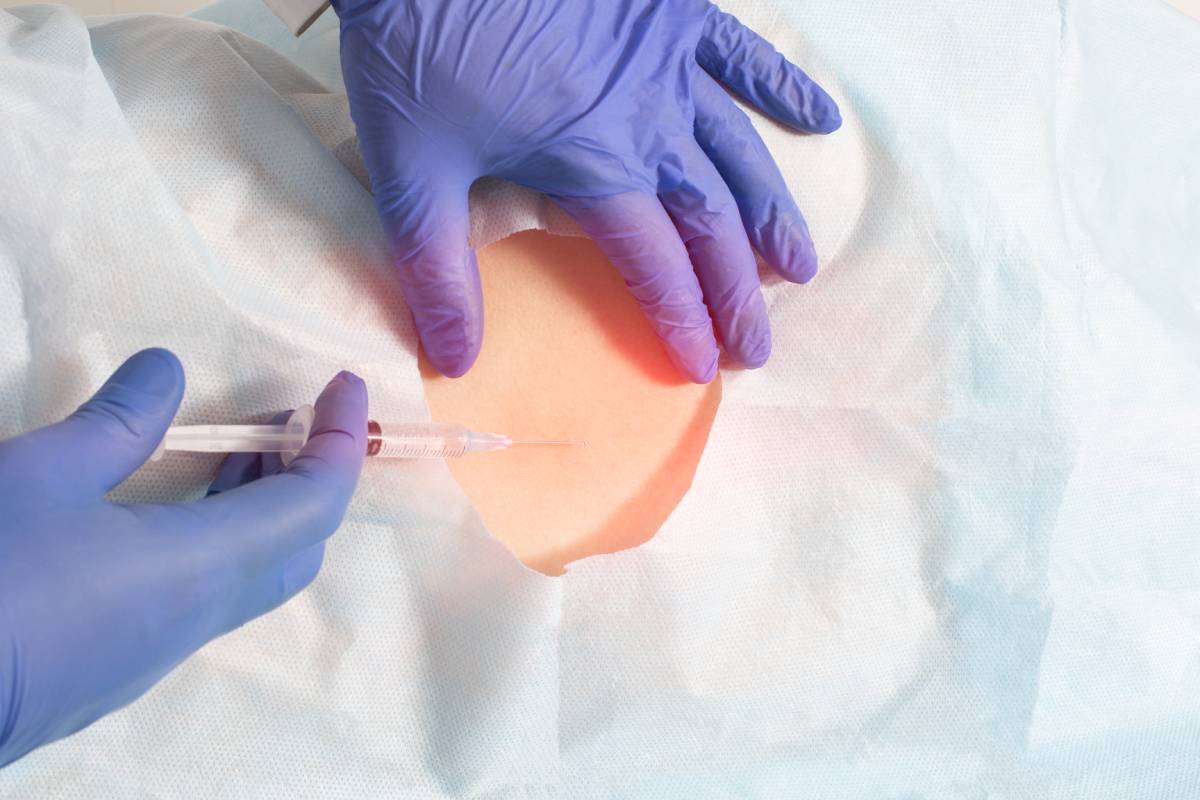
The procedure for administering spinal anesthesia involves a carefully executed lumbar puncture, typically between the L3-L4 or L4-L5 vertebrae. Patients are positioned either sitting or laterally, and strict aseptic technique is employed to prevent infection. After identifying the correct anatomical landmarks, a fine spinal needle is advanced through the dura mater. Correct placement is confirmed by the aspiration of cerebrospinal fluid, after which the anesthetic agent is injected and disseminates within the subarachnoid space.
The choice of anesthetic agent is one of the factors that influences the duration of spinal anesthesia. Commonly used agents include lidocaine, bupivacaine, and tetracaine, each with distinct duration profiles. Lidocaine provides short-duration anesthesia, typically lasting 60–90 minutes, making it suitable for brief procedures such as cystoscopies or hemorrhoidectomies. Bupivacaine offers an intermediate duration of 2–4 hours, ideal for joint replacements or hernia repairs. Tetracaine, with the longest effect lasting 4–6 hours, is reserved for prolonged surgeries like radical prostatectomies. To enhance and prolong analgesia, these agents are often combined with additives such as epinephrine or opioids.
The pharmacokinetics of spinal anesthesia are governed by several factors that determine the duration of action. The elimination half-life (t1/2) of the anesthetic agent is a key determinant, which is influenced by its volume of distribution (Vd) and clearance (Cl). This relationship is expressed by the equation:
t1/2 = (0.693 × Vd) / Cl
The volume of distribution (Vd) represents the theoretical volume in which the total amount of drug would need to be uniformly distributed to produce the observed blood concentration. In the context of spinal anesthesia, Vd is primarily influenced by the lumbosacral cerebrospinal fluid (CSF) volume, which can vary significantly between patients. Factors such as age, body habitus, and pregnancy can affect CSF volume. For instance, pregnant women tend to have a reduced CSF volume due to increased intra-abdominal pressure, potentially leading to a higher spread of anesthetic and a more pronounced effect. Clearance (Cl) refers to the volume of blood cleared of the drug per unit time. In spinal anesthesia, clearance is primarily determined by the uptake of the anesthetic by neural tissues and vascular absorption. Patient factors such as age, cardiovascular status, and spinal anatomy can influence clearance rates and therefore the duration of spinal anesthesia. For example, elderly patients may have reduced clearance due to decreased cardiac output and altered spinal blood flow, potentially prolonging the duration of anesthesia.
Lipid solubility and protein binding also play crucial roles in determining duration. Highly lipid-soluble agents like bupivacaine bind tightly to neural tissues, delaying systemic absorption and prolonging their effect. The baricity of the anesthetic solution further modulates duration. For example, hyperbaric solutions, which are denser than cerebrospinal fluid, settle into dependent spaces and concentrate near nerve roots. On the other hand, isobaric solutions diffuse more evenly, potentially prolonging sensory blockade.
The duration of spinal anesthesia is a delicate balance of drug selection, use of adjuncts, and consideration of patient physiology. A thorough understanding of pharmacokinetic principles allows anesthesiologists to tailor their approach, optimizing outcomes for a diverse range of surgical needs. As the field of anesthesiology continues to advance, future innovations such as sustained-release formulations or novel adjuvants may further enhance the controllability and efficacy of spinal anesthesia, expanding its applications and improving patient care.
References
- Dabbagh A, Dahi-Taleghani M, Elyasi H, et al. The duration of spinal anesthesia with 5% lidocaine in chronic opium abusers compared with nonabusers. Anesth Analg. 2007;105(2):531-533. https://doi.org/10.1213/01.ane.0000268496.46319.25
- Vlessides M, Kahn RL, Macaulay W, et al. Time of return of neurologic function after spinal anesthesia for total joint arthroplasty: A randomized clinical trial of 2% mepivacaine versus 0.5% bupivacaine. J Arthroplasty. 2019;34(7):1458-1464. https://doi.org/10.1016/j.arth.2019.03.035
- Soffin EM, Vaishnav AS, Wetmore DS, et al. Spinal anesthesia in awake surgical procedures of the lumbar spine: A systematic review and meta-analysis. J Neurosurg Spine. 2021;35(6):754-764. https://doi.org/10.3171/2021.6.SPINE21396
- Higuchi H, Hirata J, Adachi Y, Kazama T. Influence of lumbosacral cerebrospinal fluid density, velocity, and volume on extent and duration of plain bupivacaine spinal anesthesia. Anesthesiology. 2004;100(1):106-114. https://doi.org/10.1097/00000542-200401000-00019
- Peng PW, Chan VW, Perlas A. Minimum effective anaesthetic concentration of hyperbaric lidocaine for spinal anaesthesia. Can J Anaesth. 1998;45(2):122-129. https://doi.org/10.1007/BF03013250