Electrocardiographic (EKG) monitoring during surgery is a fundamental tool for detecting cardiac arrhythmias, myocardial ischemia, and conduction abnormalities in real time. However, the accuracy of this monitoring depends heavily on proper lead placement, which must often be adjusted to accommodate the unique anatomical and procedural demands of the intraoperative setting. Despite its routine use, the topic of optimized EKG lead placement during surgery is often overlooked.
For standard monitoring, a three-lead or five-lead EKG system is used. While three-lead setups (typically leads I, II, and III) are sufficient for rhythm monitoring, they are inadequate for ischemia detection. Five-lead systems provide a more comprehensive view and enable the placement of a precordial lead (often V5), which improves sensitivity for detecting ischemic ST changes. Monitoring leads II and V5 simultaneously has been shown to detect approximately 80% of intraoperative ischemic events. Adding lead V4 increases detection to over 90% (1).
Accurate placement of precordial leads is especially important in surgeries where the risk of myocardial ischemia is elevated. However, positioning requirements during surgery often necessitate deviations from standard EKG lead placement. In prone or lateral positioning, anterior chest leads may be inaccessible. In these cases, posterior or alternative lateral placements are used to approximate standard vectors. While not identical to conventional placements, these modified configurations can provide functionally comparable waveforms when properly aligned with the cardiac axis (2).
Pediatric surgery presents distinct challenges due to limited surface area and the concurrent use of central lines or monitoring equipment. Proper spacing and secure placement of electrodes must be balanced against maintaining surgical access. Leads are often adjusted to lateral thoracic or infraclavicular positions in such cases. These positions provide reasonable signal quality while minimizing interference with sterile fields and vascular access points (3).
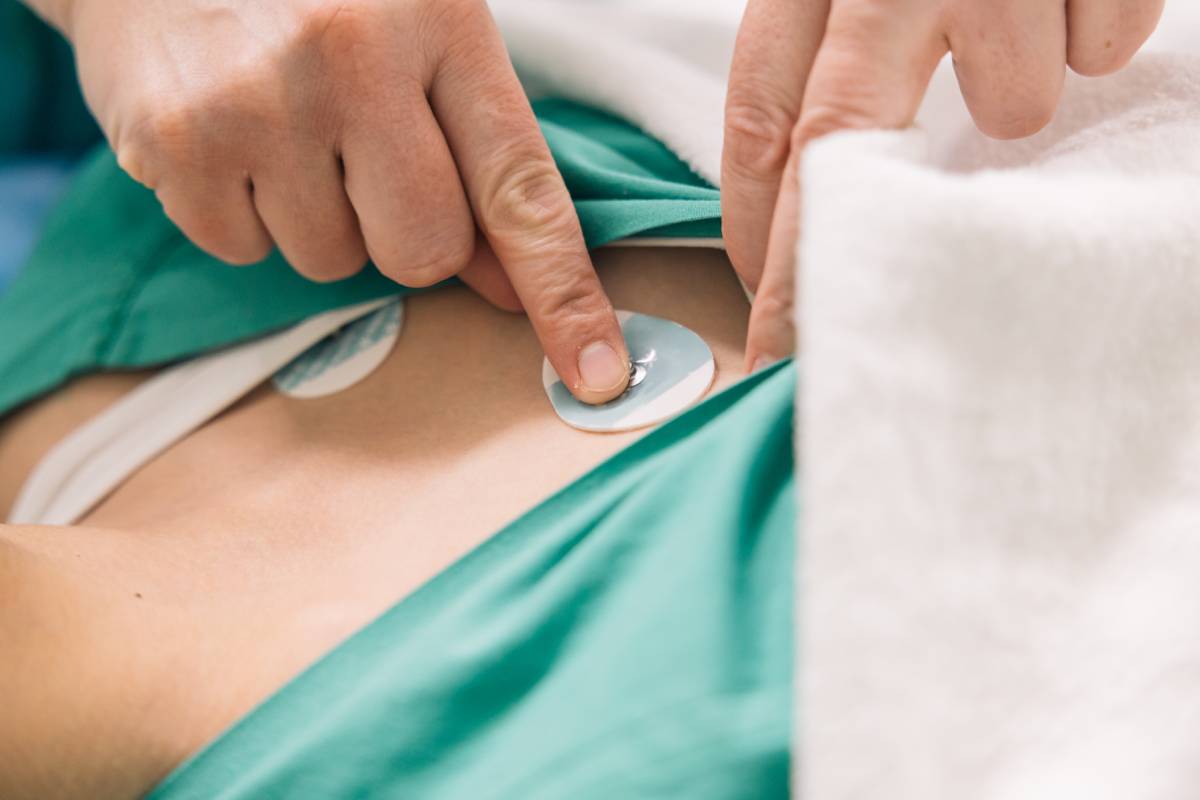
Intraoperative artifacts are another consideration. Electrocautery devices, patient warming systems, and surgical manipulations may cause transient electrical noise. Signal integrity depends on good skin-electrode contact, low impedance, and avoiding muscle groups or bony prominences. Preparing the skin with alcohol and abrasive pads, using high-quality adhesive electrodes, and employing shielded cables contributes to improved signal quality and reduced false alarms (4).
In specific cardiac procedures, the utility of lead positioning extends beyond surface monitoring. During surgery involving cardiac pacing or mapping, EKG monitoring assists in confirming effective capture or localization of electrical activity, and lead placement is particularly important. EKG guidance has been used to confirm catheter placement, optimize atrial or ventricular pacing thresholds, and guide intraoperative interventions. Newer methods, such as His-bundle pacing and electroanatomic mapping, integrate precise electrical data with anatomical positioning. This further emphasizes the need for optimal electrode configurations (5).
Despite its routine nature, EKG monitoring during surgery requires more than a passive setup. Anesthesiologists must evaluate EKG lead placement based on each patient’s anatomy, the surgical approach being used, and the risks associated with the surgery. Adjustments should be made deliberately with an understanding of how changes in placement affect signal morphology. When ischemia detection is a priority, precordial leads should be used and monitored continuously.
Proper EKG lead placement is critical to monitoring accuracy during surgery. Variations in body habitus, surgical positioning, and equipment use require clinicians to adapt while maintaining fidelity to physiological vectors. Optimizing this aspect of intraoperative care enhances the early detection of cardiac events, supports hemodynamic stability, and improves patient outcomes.
References
Pestrea C, Gherghina A, Ortan F, Cismaru G, Radu R. His bundle pacing – a curative method: A Case Report. Medicine (Baltimore). 2020;99(32):e21633. doi:10.1097/MD.0000000000021633
Mark JB. Multimodal detection of perioperative myocardial ischemia. Tex Heart Inst J. 2005;32(4):461-466.
Pawlik MT, Kutz N, Keyl C, Lemberger P, Hansen E. Central venous catheter placement: comparison of the intravascular guidewire and the fluid column electrocardiograms. Eur J Anaesthesiol. 2004;21(8):594-599. doi:10.1017/s0265021504008026
Miller JW, Vu DN, Chai PJ, et al. Upper body central venous catheters in pediatric cardiac surgery. Paediatr Anaesth. 2013;23(11):980-988. doi:10.1111/pan.12261
Silver ES, Nash MC, Liberman L. Implantation of permanent pacemaker and ICD leads in children using a three-dimensional electroanatomic mapping system as an aid to fluoroscopy. Pacing Clin Electrophysiol. 2015;38(4):448-454. doi:10.1111/pace.12579